Parathyroid Surgery
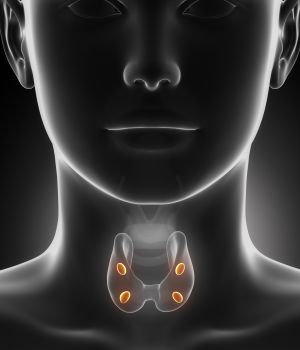 There are four small glands, called parathyroid glands, on each corner of the thyroid gland. The parathyroid glands main function is to regulate bodily calcium and phosphorous levels. This is done through the production of parathyroid hormone (PTH). When parathyroid hormone is overproduced (hyperparathyroidism), the blood calcium level becomes elevated. This can have mild to serious effects on your overall health.
There are four small glands, called parathyroid glands, on each corner of the thyroid gland. The parathyroid glands main function is to regulate bodily calcium and phosphorous levels. This is done through the production of parathyroid hormone (PTH). When parathyroid hormone is overproduced (hyperparathyroidism), the blood calcium level becomes elevated. This can have mild to serious effects on your overall health.
Conditions Treated
Hyperparathyroidism
Parathyroid Cancer
Hyperparathyroidism Symptoms
When the parathyroid produces too much PTH, abnormally high amounts of calcium are found in the blood and phosphorus drops to abnormally low levels. Generally, symptoms are minor aches and fatigue. Serious complications can develop. These include:
- Kidney stones
- Heartburn
- High blood pressure
- Increased thirst and urination
- Peptic ulcers
- Nausea
- Osteoporosis
- Poor memory
There are numerous tests that may be recommended to establish the diagnosis of hyperparathyroidism. Such tests might include: neck ultrasound and/or sestamibi (nuclear medicine) exam. A bone density test may be used to see if the imbalance has increased your risk of osteoporosis. Urine and blood tests may be needed to check for kidney function and the presence of kidney stones. If criteria for surgery are felt appropriate, surgical intervention is curative of primary hyperparathyroidism.
Hypoparathyroidism Symptoms
When too little PTH is produced, it results in unusually low calcium and unusually high phosphorus blood levels. Symptoms of hypoparathyroidism include:
- Excessive nervousness
- Headaches
- Muscle cramps
- Unwanted muscle contraction resulting in uncontrollable twitching and convulsions
- Seizures
Calcium may need to be administered through an IV in order to decrease muscle spasms in severe cases. Long term treatment includes calcium and vitamin D supplements. In addition, a calcium-rich and low-phosphorus diet is recommended.
Parathyroid Surgery
Parathyroid disease is usually treated with a minimally-invasive procedure (MIP) under a light or general anesthetic. Intra-operative parathyroid hormone is monitored to ensure adequate removal of the abnormal gland(s). This is usually performed in the outpatient setting. The smaller incisions result in quicker recovery and shorter convalescence. Approximately 85% of the time, only one of the four parathyroid glands needs to be removed. This is the result of a benign (non-cancerous) growth on the gland called an adenoma. In approximately 10% of cases, all four glands are enlarged and over producing parathyroid hormone. Either 3½ glands are removed or all 4 are taken out with replacing a portion of one of the glands in the neck or arm muscle. This allows it to regenerate and gain normal parathyroid function over time. This is called a parathyroid auto-transplantation.
Getting Back to Normal
- Your incision is closed with a dissolvable suture. A paper bandage will be directly covering the wound. This will be removed at your follow-up visit. You may shower the day after surgery. Your incision will be firm, pink and raised over the next couple of weeks. This will eventually soften. Mild bruising is to be expected over the lower neck or upper chest. This will resolve without further concern. You may experience neck pressure or tightness when swallowing for the first couple of months. This will completely resolve.
- You may resume normal activities after one week. No strenuous activity for the first week. Delayed bleeding complications can occur. If you experience any significant new swelling or pain, call the office immediately.
- Pain should be minimal after your procedure. Post-operative complaints generally consist of pain with swallowing or a neck ache. Pain is often adequately controlled with ibuprofen (400-600mg) or Tylenol (650mg) every 4-6 hours as needed. If these medications are not sufficient, do not hesitate to use the narcotic pain pills as prescribed. Be sure to use an over the counter stool softener such as Colace or Docusate if using prescription pain medications.
- Your voice will often appear hoarse immediately after surgery. Other patients experience voice “fatigue” at the end of the day. This will usually resolve within 2-3 months.
- Hypocalcemia (low calcium level) is a common temporary complication of thyroid or parathyroid surgery. Symptoms may include numbness or tingling around your lips or in your fingertips. Some patients may experience muscle twitching, headache or “skin crawling”. This will usually occur within 2-3 days after surgery. Treatment is with either 2 regular strength (500mg) Tums tablets 3 times daily OR 1 Ultra strength (1000mg) Tums Tablet 3 times daily. Have these on hand prior to returning home from the hospital. Please notify the office if you experience these symptoms. If symptoms do not resolve with Tums, call the office and have the physician paged at 303.449.3642.These symptoms should resolve within 7-10 days. Levels will be checked periodically after surgery.
- Thyroid supplementation – if you were taking thyroid supplementation prior to surgery, continue your current dose unless instructed. Otherwise, if you were not taking thyroid hormone prior to surgery, you may be given a new prescription. Thyroid hormone levels will usually be checked 4-6 weeks after surgery. Levels often do not stabilize for up to 6 months after surgery.
- If you experience fever greater than 101 degrees Fahrenheit, chills,or any drainage other than a thin red fluid, please call the office at 303‑449‑3642.
- DRIVING MAY RESUME WHEN OFF ALL NARCOTIC PAIN medications and you can turn or twist your body without hesitation. Do not hesitate to move your head after surgery.
- Schedule a post-operative visit 7-14 days after surgery if one has not been arranged before surgery. Please call the office at 303‑449‑3642.
